By Sadie Lipe
Depressed? Anxious? You’re not alone.
The National Alliance on Mental Illness-Chicago (NAMI-Chicago), a nationwide organization which provides mental health resources and support to the public, estimates approximately 5 million Illinois adults have poor mental health. 2.1 million more people are living with a mental illness and 434,000 have a serious mental condition.
Depression, anxiety and other mental health issues have a variety of causes. New research is showing that one of the culprits may be something long overlooked – unhealthy diets.
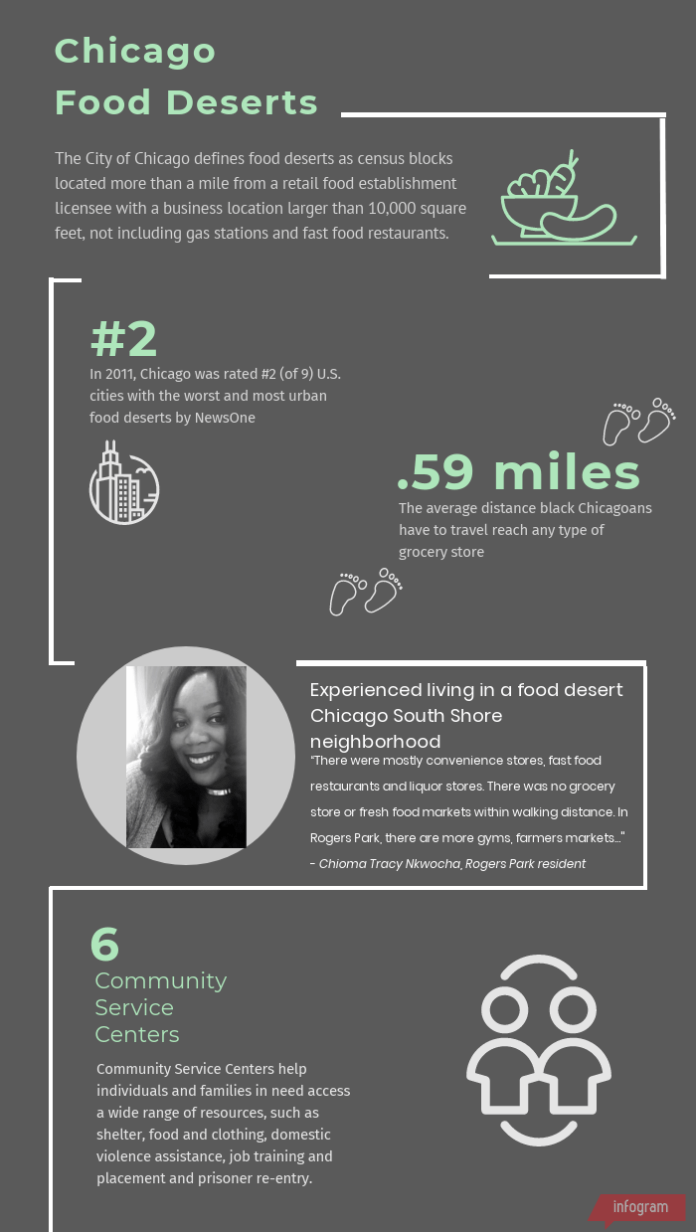
But adding more fruits and vegetables isn’t easy for the Chicagoans who live in food deserts, neighborhoods without grocery stores. Others can’t afford fresh produce.
A slew of recent studies have found that in areas with few healthy food options, mental health issues are extremely high.
Chicago’s Food Deserts
In Chicago, more than 600,000 people – 22% of the city’s residents – don’t have access to fresh fruits and vegetables, according to city’s data portal.
10 of the city’s 50 wards meet the government’s definition of “food desert.”
According to the U.S. Department of Agriculture, a food desert is an area in which 20 percent of the residents live in poverty, and where at least a third of the population in lives more than a mile from a supermarket or large grocery store.
What Newer Discoveries are Telling Us
A recent compilation of 21 studies found “a dietary pattern characterized by high intakes of fruit, vegetables, whole grain, fish, olive oil, low-fat dairy and antioxidants, and low intakes of animal foods was apparently associated with a decreased risk of depression.”
Much of the new research focuses on a person’s gut biome.
“Current research is finding that gut bacteria control everything from sugar cravings — bacteria feed on sugar — to depression, anxiety, Attention Deficit Hyperactivity Disorder (ADHD) and most other mental health disorders,” says Marla Brodsky, a registered nutritionist and owner of Luscious Life Nutrition in Rogers Park. “A disproportion of bad bacteria versus healthy bacteria can create inflammation in the brain and affect its health and function.”
Brodsky added there is a growing amount of research on how probiotics, prebiotics, limiting processed and refined carbohydrates and consuming essential fatty acids, such as fish oil and coconut oil, can improve brain function and mental health disorders ranging from depression, anxiety, Attention Deficit Disorder (ADD), schizophrenia and autism.
Virginia Mansuy Aubert, assistant professor in Loyola’s Department of Cell and Molecular Biology and Division of Neurosciences, said much of this research is still under active debate.
“Some data has been published which shows gut bacteria are indirectly involved in the production of dopamine or serotonin,” Aubert said.
Dopamine and serotonin are neurotransmitters, or chemical compounds, produced in the brain and the intestines. Both are believed to help regulate mood and social behavior, appetite, digestion sleep and memory.
Although there is no clear conclusion on what causes depression, a key theory is it might involve an imbalance of neurotransmitters and hormones in the body. Depression has been linked to low levels of serotonin, and lower levels of serotonin have been found to cause poor memory, distressed mood, difficulty sleeping, low self-esteem, anxiety and aggression.
Everyday emotional well-being relies on messages sent from the neurotransmitters located in the gut to the brain. As a result, changes in the gut microbiome can directly impact the levels of serotonin and dopamine produced for the brain, according to Aubert.
The Second Brain
The main center for the stomach’s “second brain” is connected with the larger one in our skulls. Daily nutrition quality and intake partly determines the health of this second brain and plays key roles in preventing or exacerbating mental health issues, according to Aubert.
The biological term for the second brain is the enteric nervous system. The enteric nervous system consists of neurons embedded in the walls of the long tube of the gut, which is roughly nine meters long. This nervous system also contains about 100 million neurons, which is more than in the spinal cord or peripheral nervous system.
Aubert said the enteric system’s neurons communicate the gut’s status to the brain via the vagus nerve. Through this pathway, the gut can change neurotransmitter levels in the brain, in affect changing one’s behavior.
Medical and nutritional experts, along with Aubert and Brodsky, recommend diets heavy in plant fibers as these fibers ferment in the gut and help regulate the gut’s diverse bacteria.
Brodsky recommends eating a diet rich in brightly colored plant foods for their antioxidant effects, high quality protein, such as cold water fish and grass fed meats, healthy fats from olive oil, coconut oil, avocado, nuts and seeds, and to avoid sugars, processed flours and carbohydrates.
But achieving these dietary recommendations can be difficult, especially for those who can’t find them located relatively to their homes, or within a price point which fits their financial capabilities.
Personal Stories
For one Rogers Park resident, leaving a food desert allowed her to notice a drastic difference in her mental health and mood after moving out of a food desert located in Chicago’s South Shore neighborhood.
“There were mostly convenience stores, fast food restaurants and liquor stores. There was no grocery store or fresh food markets within walking distance. In Rogers Park, there are more gyms, farmers markets … I can take a walk, and it’s more bike and pedestrian family,” Chioma Tracy Nkwoch says.
Thinking back to when he and his family lived in a food desert, another resident of the Edgewater area said it became nearly impossible to tolerate, and he could feel the effects trickling down to his children.
“All my kids knew was going through the drive-thru, or stopping at some run-down mini mart on the way home from school to grab something to eat for dinner. And at those mini marts, prices for produce, which was often not in the best condition or expired, was expensive,” said Mark Kaswacalski.
A single father raising three children, Kaswacalski used to reside on the outer edges of Garfield Ridge near Chicago’s southwest side. But after landing a better paying job farther north in the city, Kaswacalski was able to move his family to Edgewater.
“Now we can shop at Aldi, Jewel Osco or if we’re feeling fancy, we can look around in Whole Foods,” Kaswacalski added. “My children seem much happier, which makes me much happier. Moving here has put us in a better mood overall and made our lifestyles more healthy.”
Both residents said they’re able to cook at home more often after leaving their food deserts, with Kaswacalski adding his children now bring packed lunches to school instead of eating the “inedible lunches” served at their old schools in Garfield Ridge.
“The kids feel like they have more of a say [in what they get to eat] and they even help me pick out what they want for lunch and dinner when we go grocery shopping,” Kaswacalski said.
However, healthy food prices still vary from store to store and by what’s in season. Factors, such as distance traveled from farm to store, organic versus conventional and discounts applied from customer reward programs, can all affect prices.
Where do we go from here?
Having the freedom to choose what to eat from the multitude of options in non-designated food deserts leaves room for dietary experimentation and progress toward a healthier lifestyle and, ultimately, a happier mind.
“It has been a while that we’ve known that to have good mental health, it’s necessary to treat the body well by eating healthy and moving around … helping our gut friends be happy lets our gut, mind and spirit live in good harmony,” Aubert said.
Quiz yourself!
Think you know all about healthy foods? Show us your stuff. Take this short quiz to test your food IQ.
















